Introduction
High-hyperdiploidy (HHD) represents the most common cytogenetic abnormality found in B-cell precursor acute lymphoblastic leukemia (B-ALL). Despite the overall good outcome of this entity, up to 15% of patients suffer from disease relapse. Genome-wide ALL studies with next-generation sequencing (NGS) approaches identified a distinct pattern of somatic mutations in HHD ALL, enriched in mutations occurring in genes activating the RAS pathway and in CREBBP gene, especially in relapsed patients.
Although several studies have attempted to explore the prognostic significance of these mutations that are potentially susceptible of targeted therapies, their impact in uniformly treated patients with newly diagnosed B-ALL is not well characterized, and there is no consensus on their clinical significance. In this study, we aimed to investigate the frequency of recurrent mutations and to define their prognostic role in the setting of newly diagnosed HHD B-ALL, by using end of induction minimal residual disease (MRD) and event-free survival (EFS).
Methods
We included 101 consecutive patients, aged between 1-17 years, with newly diagnosed HHD B-ALL and enrolled in the AIEOP-BFM ALL 2009 protocol (NCT01117441). HHD was defined by the presence of a DNA index ≥1.16 and lack of ETV6::RUNX1, BCR::ABL1, KMT2A::AFF1 translocations.
Diagnostic leukemia samples of 89 patients were sequenced using a validated clinical NGS panel profiling 39 genes involved in leukemia pathogenesis. Mutations affecting RAS pathway ( NRAS, KRAS, PTPN11, NF1, BRAF) and mutations affecting CREBBP gene were included. In addition, digital multiplex ligation-dependent probe amplification (digital MLPA) analysis for the identification of IKZF1 deletion and IKZF1plus phenotype was evaluable for 67 patients.
A Fisher exact test and Wilcoxon rank sum test were used for categorical and continuous variables. MRD was assessed by an IG/TR PCR assay at day +33 of induction (timepoint 1, TP1) and at day +78 (timepoint 2, TP2). EFS was estimated by using Kaplan and Meier method and differences between groups were tested using the log-rank test. Resistance to treatment, relapse, death or second malignant neoplasm were considered as events, whichever occurred first.
Results
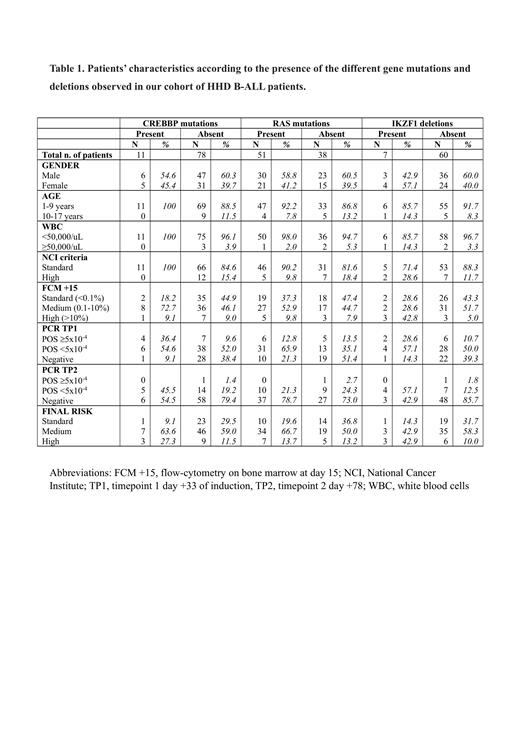
Patients' characteristics according to the presence of studied mutations are shown in Table 1. Mutations affecting RAS pathway and CREBBP occurred in 57.3% and 12.3% of HHD B-ALL patients, respectively. Clonal RAS pathway mutations, defined by variant allele frequency (VAF) ≥25%, were found in 16.8% of cases. Among the 11 patients with mutations of CREBBP, 7 had also a mutation affecting KRAS and the association was significant (p=0.03). Seven patients (10.4%) had deletion of IKZF1, of whom 5 (7.4%) were IKZF1plus. There was no association between any mutations or IKZF1 status and patient presenting characteristics, as including sex, age and WBC counts.
MRD was evaluable in 84 patients at the end of induction (TP1). MRD level ≥5x10 -4 was found in 36.4% of patients with CREBBP mutations and in 9.6% of those without, and this association was statistically significant (p=0.02). Additionally, MRD negativity was found in 9.1% and 38.4%, respectively. At TP2, MRD was still detectable in 45.5% of patients with CREBBP mutations compared to 20.6% of those with CREBBP wildtype (p=0.08).
Similarly, we observed an association between RAS pathway mutations and MRD at TP1 (p=0.01) with a marked difference in MRD negative patients (21.3% vs 51.4% in patients with and without mutations). No association was observed between MRD level and clonal RAS pathway mutations or IKZF1 status.
Despite the association between CREBBP mutations and high MRD at TP1, no significant difference in final high-risk group was found (27.3% vs 11.5%, p=0.17).
A total of 8 events were observed, of which 6 were relapses. No impact of any mutations or IKZF1 status in term of 5-years EFS was found in our cohort.
Conclusion
Our study shows that CREBBP mutations in HHD B-ALL are associated with inferior early response to treatment in terms of MRD level at the end of induction (TP1) but not with worse EFS with our whole current chemotherapy backbone.
Therefore, the inclusion of CREBBP mutated patients in very low risk protocols should be carefully evaluated.
The validation of these findings is ongoing through the analysis of patients treated by other international study groups adopting different chemotherapy backbones.
Disclosures
Rizzari:CLINIGEN, JAZZ, SERVIER, SERB: Consultancy, Honoraria, Speakers Bureau. Biondi:Colmmune: Membership on an entity's Board of Directors or advisory committees, Research Funding; Galapagos: Membership on an entity's Board of Directors or advisory committees; Agmen: Speakers Bureau; Novartis: Speakers Bureau; BMS: Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal